50/M FEVER COUGH WITH SPUTUM,UNCONTROLLED SUGARS
CHIEF COMPLAINTS
HOPI
Fever since 15-days high grade-not associated with chills and rigor, evening rise + Associated with sweating
Cough since 7- days associated with less amount of sputum, mucoid. blood tinged aggravated on changing position from lying down to sitting position, no reliving factors
SOB grade - I MMRC -: 7 days more associated with cough, relieved on rest not associated with wheeze
H/o RTA 1 1/2 year back
Fracture of neck of femur with dynamic hip screw surgery done in outside Hospital.Immobilisation 1 month to 1-1/2 year back
Patient is Binge Alcoholic and Smokes 18 cigarettes in a day later he started smoking Bedi Suttas(high tobacco cigar) in day.
Patient attendant said that their neighbour has TB ( who is son in law of him )
And Patient visits weekly 4 times to his home & spend with him approximately 1-hour a day
Patient started to have fever since 10 days at night time with burning sensation all over the body
Patient started to have unbearable pain at lower back during cough .and always needed help from attendants to hold his back during coughing.
PAST HISTORY
K/c/o DM since 2 years was diagnosed during his RTA treatment and is on regular Glimipride 1mg &Metformin 500mg medication since then.
He has no history of hypertension, diabetes ,asthma, epilepsy, tuberculosis.
GENERAL EXAMINATION
Patient is conscious, cooperative ,coherent and oriented with time , place , date.
Slightly pallor,
No icterus, cyanosis, clubbing, lymphadenopathy, edema was noted
VITALS:
Bp-80/40 mm Hg
Pr-102 bpm
Rr-25 cpm
Temperature:99.5
Spo2: 98%@RA
GRBS- HIGH
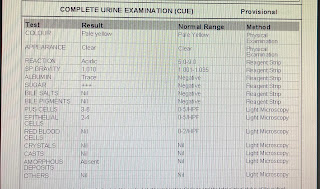
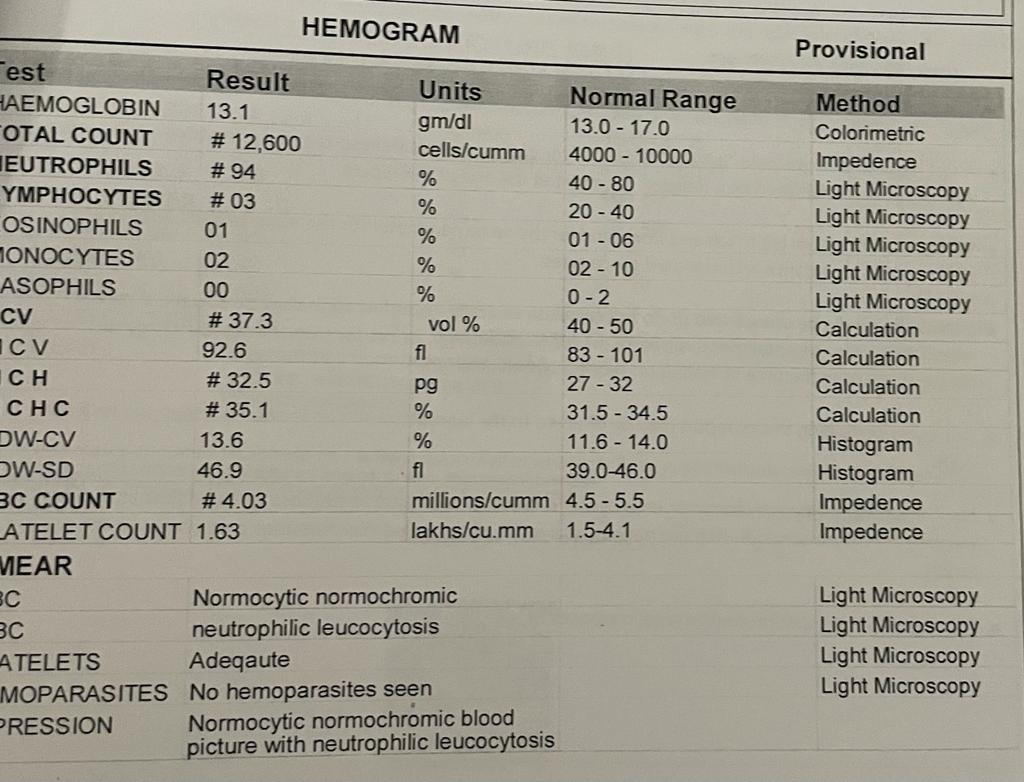
INVESTIGATIONS
SYSTEMIC EXAMINATION
CVS:S1 S2 heard , No murmurs
CNS:
No focal neurological deficit
RS:
Breath movements -abdominal thoracic
In infra scapular area of left lung
Inspection: chest shape normal,
Dysponea - present
Palpation: trachea -central
Auscultation: basal crepitations are heard